Intermittent fasting has become a buzzword in health and nutrition circles. While it’s often associated with weight loss and metabolic health, many people are now exploring its potential benefits for blood sugar control and managing type 2 diabetes.
So, what does the science really say? Can this eating pattern help you manage diabetes more effectively—or even reverse it? And is it safe?
This article explores how intermittent fasting may impact blood sugar, insulin sensitivity, and overall health for people with diabetes. We’ll also look at risks, real research, and practical tips for getting started.
What Is Intermittent Fasting?
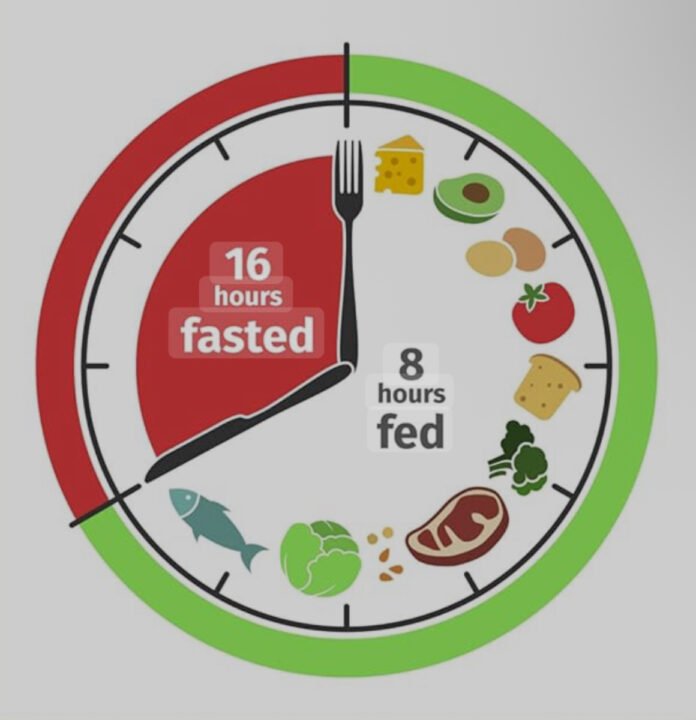
Intermittent fasting (IF) isn’t a diet—it’s a way of scheduling meals. Instead of eating throughout the day, you limit food intake to a specific time window and fast during the remaining hours.
Popular methods include:
- 16/8: Fast for 16 hours, eat in an 8-hour window (e.g., 12 p.m. – 8 p.m.)
- 5:2: Eat normally for 5 days, restrict calories to 500–600 on 2 non-consecutive days
- Alternate-Day Fasting: Eat every other day or follow a reduced-calorie plan on fasting days
- OMAD (One Meal A Day): All daily calories consumed in one sitting
Each method can be customized based on personal health goals and lifestyle.
How Fasting Affects Blood Sugar and Insulin
Intermittent fasting can have a significant impact on two key aspects of diabetes management: blood sugar levels and insulin function. During fasting periods, the body shifts from using food for energy to tapping into stored glucose and fat. This metabolic switch can help reduce insulin levels and improve how the body responds to insulin over time.
In people with type 2 diabetes, insulin resistance is a core issue. The body produces insulin, but cells become less responsive, making it harder to regulate blood glucose. Fasting helps “rest” the system by lowering insulin levels during non-eating periods, allowing insulin sensitivity to improve gradually.
Studies show that fasting can reduce both fasting glucose levels and HbA1c, which is the long-term marker for blood sugar control. These improvements often occur alongside weight loss, particularly in abdominal fat—a key contributor to insulin resistance.
Fasting may also reduce post-meal blood sugar spikes by enhancing the body’s ability to process glucose more efficiently. However, individual responses can vary, and close monitoring is essential—especially for those on insulin or glucose-lowering medications.
When approached safely, intermittent fasting can offer meaningful metabolic benefits and support better glucose management in people with type 2 diabetes.
Key Benefits Observed in Studies:
- Improved insulin sensitivity: Cells become more responsive to insulin, making blood sugar easier to manage.
- Lower fasting glucose levels: Fasting periods can help reduce both immediate and long-term blood sugar readings.
- Reduced abdominal fat: Visceral fat, which contributes to insulin resistance, tends to decrease with intermittent fasting.
Did you know? A study in Cell Metabolism showed that early time-restricted eating improved insulin sensitivity—even without weight loss.
What the Research Says
The scientific interest in fasting as a tool for managing type 2 diabetes has grown significantly in recent years. While larger, long-term studies are still needed, several small trials and case reports suggest that intermittent fasting may offer meaningful benefits for blood sugar regulation and metabolic health.
One of the most cited examples comes from a 2019 BMJ Case Reports study, where three men with type 2 diabetes were able to discontinue insulin therapy after practicing intermittent fasting under medical supervision. Each patient saw improved glucose levels, better energy, and weight loss—all without complications.
Another notable trial, published in Nutrition and Healthy Aging (2018), showed that time-restricted eating—without any calorie restriction—led to lower fasting glucose and insulin levels in overweight individuals. Importantly, these improvements happened even when no weight loss occurred, highlighting the metabolic power of meal timing alone.
Additionally, a 2021 study in the Journal of Clinical Endocrinology found that fasting protocols reduced inflammatory markers and improved insulin sensitivity in adults with prediabetes.
While the results are encouraging, it’s clear that any fasting plan must be approached with care—especially for individuals using diabetes medications. Still, the early science offers strong support for structured eating schedules as a promising strategy in diabetes care.
Highlights:
- BMJ Case Reports (2019): Three individuals with type 2 diabetes were able to stop insulin therapy after using intermittent fasting under medical supervision.
- Nutrition & Healthy Aging (2018): Participants practicing time-restricted eating experienced reductions in insulin and blood sugar levels.
- Journal of Clinical Endocrinology (2021): Fasting protocols reduced inflammation and improved metabolic markers in adults with prediabetes.
⚠️ Is It Safe for Everyone?
Fasting isn’t suitable for all people living with diabetes—especially those on certain medications.
⚠️ Use Caution If You:
- Take insulin or sulfonylureas
- Have type 1 diabetes
- Are pregnant or breastfeeding
- Have a history of disordered eating
- Struggle with low blood sugar episodes (hypoglycemia)
📞 Tip: Always consult your doctor before starting a fasting regimen if you’re managing diabetes or using blood sugar–lowering medication.
How to Get Started Safely
If you’re curious about trying time-restricted eating as part of your diabetes care plan, start slow and stay consistent. Here are some safe steps:
✅ 1. Ease Into It
Try a 12-hour fast (e.g., 8 p.m. to 8 a.m.) for a few days. Gradually increase to 14 or 16 hours as your body adjusts.
✅ 2. Prioritize Nutrient-Rich Meals
During eating windows, choose foods that help stabilize blood sugar:
- Lean protein (chicken, eggs, tofu)
- Low-glycemic carbs (quinoa, lentils, oats)
- Healthy fats (avocado, olive oil, almonds)
- Fiber-rich veggies (spinach, broccoli, bell peppers)
- Fruits in moderation (berries, apples)
✅ 3. Monitor Blood Sugar Closely
Track glucose levels more frequently during the first few weeks to avoid unexpected lows or spikes.
✅ 4. Hydrate Generously
Stick to water, herbal teas, or black coffee (if tolerated) during fasting periods. Avoid sugary drinks or juices.
✅ 5. Adjust Medications if Needed
Work with a healthcare provider to fine-tune medication timing or dosage, especially if your eating window changes significantly.
What to Eat During Your Eating Window
The success of any fasting plan depends largely on what you eat once you break your fast.
👍 Good Choices:
- Complex carbs (sweet potatoes, brown rice)
- Plant-based proteins (beans, lentils, tempeh)
- Whole fruits with fiber (berries, oranges)
- Fermented foods (yogurt, sauerkraut, kimchi)
- Green smoothies with minimal added sugar
👎 Avoid:
- Refined carbs and white bread
- Sugary beverages or processed snacks
- Fried or high-sodium foods
- Fast food meals
Pair It with Other Healthy Habits
Fasting alone won’t solve everything. To maximize benefits for blood sugar control, consider combining your eating plan with:
- Daily physical activity (walks, strength training)
- 7–9 hours of sleep each night
- Stress management (yoga, breathwork, journaling)
- Avoiding alcohol and smoking
All of these can reinforce metabolic improvements and help prevent diabetes complications long-term.
Frequently Asked Questions
❓ Can intermittent fasting help reverse type 2 diabetes?
For some individuals, intermittent fasting may lead to remission of type 2 diabetes—especially when paired with sustained weight loss, regular exercise, and medical supervision. While it’s not a cure, it can significantly improve blood sugar control and reduce dependence on medications.
❓ Is intermittent fasting better than counting calories?
For many people, yes. Intermittent fasting focuses on when you eat rather than obsessing over every calorie. This time-based approach reduces decision fatigue and can feel more intuitive and easier to maintain compared to traditional calorie-restriction diets.
❓ Is fasting safe for people with type 1 diabetes?
Fasting is generally not recommended for those with type 1 diabetes unless under strict medical supervision. The risks of hypoglycemia and diabetic ketoacidosis are significantly higher in this group, making unsupervised fasting potentially dangerous.
❓ Will I lose muscle fasting?
Not likely. As long as you consume enough protein during eating windows and engage in regular physical activity (especially resistance training), your muscle mass should remain intact. In fact, short-term fasting is often muscle-sparing compared to prolonged calorie restriction.
❓ Can intermittent fasting work without weight loss?
Yes. While weight loss often enhances blood sugar control, studies show that intermittent fasting can improve insulin sensitivity and glucose levels even in the absence of weight loss. The timing of meals alone can positively impact metabolic health.
❓ How soon can I expect to see results?
Some individuals notice improvements in energy, digestion, or glucose readings within a few weeks. However, meaningful changes in HbA1c or insulin sensitivity typically take 8–12 weeks. Consistency and pairing fasting with healthy meals are key.
❓ Do I need to fast every day?
Not necessarily. Many people with diabetes benefit from fasting 3–5 days per week using methods like 16/8 or 14/10. Others follow alternate-day fasting. Choose a schedule that feels sustainable and doesn’t cause fatigue or hypoglycemia.
❓ Can I drink coffee while fasting?
Yes—black coffee is generally allowed during fasting windows. It contains minimal calories and may even enhance fat burning and appetite control. Just skip sugar, cream, or high-calorie flavorings.
❓ Is intermittent fasting safe for seniors with type 2 diabetes?
It can be, but extra caution is needed. Older adults may be more sensitive to blood sugar drops, so they should start with shorter fasting windows and consult a doctor or dietitian for tailored advice.
❓ What if I feel dizzy or shaky during a fast?
These may be signs of low blood sugar (hypoglycemia), especially if you’re on medication. Break your fast immediately with a balanced snack and track your glucose. Always consult your provider before continuing with fasting.
✅ Final Thoughts
The growing interest in time-restricted eating is more than just a trend—it’s a sign that people are looking for sustainable, science-backed solutions to manage chronic conditions like type 2 diabetes. While not a cure, intermittent fasting can be a valuable tool when integrated thoughtfully into a broader health plan.
For individuals navigating blood sugar issues, especially those with type 2 diabetes, the appeal of fasting lies in its simplicity. Instead of obsessing over calorie counting or rigid meal plans, you’re focusing on when to eat—allowing your body a structured break from food intake. This approach gives your insulin levels time to fall, encourages your body to use stored energy more efficiently, and may gradually improve glucose regulation.
However, like any wellness strategy, it’s not one-size-fits-all. Fasting can yield benefits such as reduced inflammation, improved insulin response, and abdominal fat loss, but only when practiced safely and paired with proper nutrition. People managing diabetes must be especially cautious. If you take insulin or other glucose-lowering medications, starting a fasting regimen without medical guidance could increase your risk of hypoglycemia.
That’s why professional support matters. Before you make any significant shifts in your eating routine, talk to a healthcare provider or registered dietitian—especially if you’re adjusting medication, struggling with unpredictable blood sugar levels, or have other health conditions.
What’s encouraging is the growing body of research showing that fasting—when paired with balanced, nutrient-rich meals—can help many people with type 2 diabetes achieve better metabolic outcomes. Lower fasting glucose, reduced HbA1c, and even remission in some cases have been documented in early trials. But remember: those results usually come from combining fasting with healthy food choices, movement, and regular monitoring.
If you’re just starting out, begin with a gentle fasting window (like 12/12), track how your body responds, and slowly work toward longer fasting periods if appropriate. Focus your meals around high-fiber vegetables, lean proteins, and whole-food carbohydrates. Stay hydrated, manage stress, and sleep well—these are just as important as your eating window.
Also, keep in mind that consistency is key. Skipping breakfast once in a while or eating late at night occasionally won’t make or break your health—but long-term habits will. Choose a schedule that fits your lifestyle and doesn’t feel like punishment. That’s the only way any plan becomes sustainable.
In summary, intermittent fasting can support your diabetes journey, but it should be viewed as a complementary tool, not a stand-alone solution. With mindful planning, guidance from professionals, and a commitment to overall wellness, many people are finding that fasting not only simplifies their routine but empowers them to take control of their health—on their own terms.
You don’t have to be perfect. You just have to be consistent, intentional, and informed.
📌 Quick Summary
✔️ May reduce insulin resistance
✔️ Helps lower blood glucose and HbA1c
✔️ Supports belly fat reduction
✔️ Needs doctor supervision if on medication
✔️ Not for type 1 diabetes or pregnancy
✔️ Works best with a healthy, whole-food diet
🔔 Ready to Take Control of Your Blood Sugar?
Intermittent fasting could be the lifestyle change that transforms your diabetes journey. But the key to success is doing it safely and intentionally.